Pros and Cons of AI in Healthcare: Benefits, Risks, and Real-Life Use Cases
Currently, 4.5 billion people lack access to essential healthcare services, with projections forecasting a shortage of 11 million health workers by 2030.
However, the healthcare sector continues to lag in AI adoption, as noted in a World Economic Forum report. This delay may stem from healthcare professionals’ limited awareness of AI’s benefits and effective strategies for mitigating implementation risks. Based on our research, the pros and cons of AI in healthcare are the following:
- Pros of AI in healthcare: enhanced diagnostic speed and accuracy, personalized treatment planning (20-30% improvement in care relevance), administrative efficiency (40x faster documentation summarization and scribing), predictive analytics for early disease detection, accelerated drug discovery, enhanced surgical precision (21% fewer errors), continuous remote monitoring (30% reduction in readmissions), and seamless integration with traditional medicine practices.
- Cons of AI in healthcare: high implementation costs, data privacy risks, algorithmic opacity, systemic bias, workflow disruption, regulatory uncertainty, fragmented data quality, and alert fatigue. These challenges require specialized solutions like HIPAA-compliant architectures, bias detection, and intelligent alert optimization professional AI consulting agencies.
What are The Pros and Cons of AI in Healthcare?
By examining the pros and cons of AI in healthcare, stakeholders can gain a clearer understanding of its dual impact on patient care alongside the hurdles like costs and data concerns.

Below is a summarized comparison table that highlights the key advantages and disadvantages of AI technologies in the medical field.
Now, let’s explore these ideas in greater detail.
What are Pros of Using AI in Healthcare?
1. Enhanced Diagnostics Speed and Accuracy
AI algorithms can detect subtle patterns in scans that might be missed by radiologists. This leads to faster treatment decisions and better patient outcomes.
Real-life example: The AI software developed by Imperial College London, Technical University of Munich, and Edinburgh University is proven to be twice as accurate as human professionals in examining brain scans. It also can identify the stroke timescale within 4.5-6 hours.
Another instance is Massachusetts General Hospital’s collaboration with MIT, where AI achieved 94% accuracy in detecting lung nodules in X-rays and CT scans.
2. Improved and Personalized Medical Decisions
AI enables tailored treatment plans by integrating genetic, lifestyle, and clinical data to predict individual responses to therapies. AI-powered decision-making also shifts healthcare from a one-size-fits-all model to precision care.
Real-life example: Implementation of AI-driven treatment plans, one of Riseapps’ clients saw an increase in accuracy and relevance of care plans by 20-30%.

3. Administrative Efficiency
AI automates routine administrative tasks such as scheduling, billing, and documentation. For example, AI medical summarization software developed by Riseapps for one of the clients, shows that medical documentation can be summarized 40x faster compared to traditional methods. Thanks to this implementation, clinicians could focus on patient care and reduce burnout.
By handling data entry and optimizing workflows, AI cuts down on errors and wait times, leading to cost savings and improved operational efficiency.
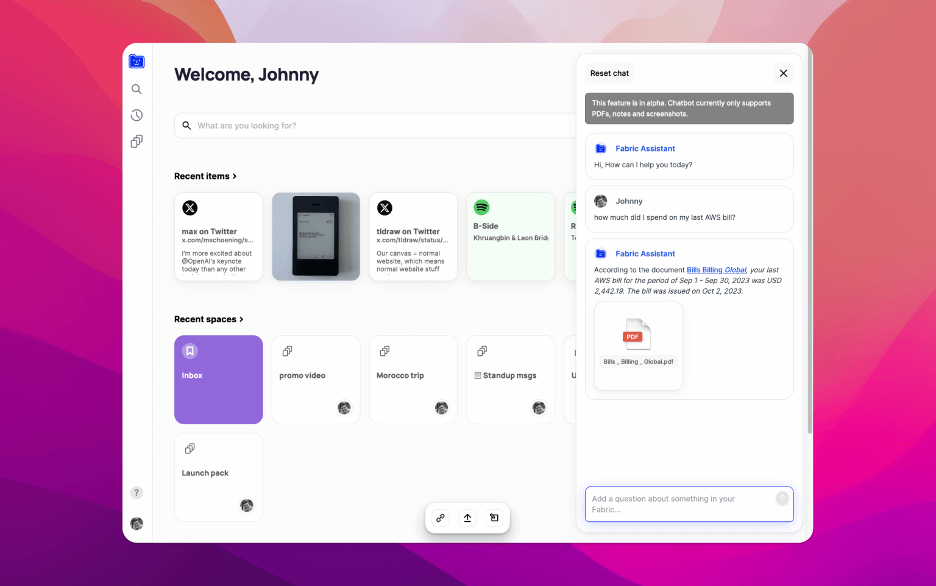
Real-life example: OSF HealthCare’s partnership with Fabric deployed the AI virtual assistant Clare, achieving $1.2 million in contact center savings and a similar increase in patient revenue.
4. Predictive Analytics and Early Disease Detection
AI uses predictive models to forecast disease risks and outcomes by analyzing historical and real-time data that result in proactive interventions that prevent complications. AI capability extends to epidemic prediction and identifying early signs of over 1,000 diseases, enhancing public health responses and individual care.
Real-life example: AstraZeneca’s AI model, trained on data from 500,000 UK individuals, predicts diagnoses like Alzheimer’s years in advance, enabling early management.
5. Accelerated Drug Discovery and Clinical Trials
AI revolutionizes drug development by predicting protein structures, suggesting new compounds, shortening timelines from years to months. In clinical trials, AI enhances patient recruitment, safety monitoring, and outcome simulations, boosting success rates.
Real-life example: The launch of Xaira Therapeutics, backed by $1 billion, uses AI to generate new therapeutic molecules, accelerating development as per OECD reports. And thanks to generative-AI-driven molecular modeling, over 70 drugs are already in clinical trials.
6. Enhanced Telesurgical Precision
AI-integrated robotic systems enhance surgical precision through real-time image analysis and tissue recognition, minimizing invasiveness and recovery times. This reduces complications and human fatigue, making complex procedures safer, especially in pediatrics and specialties like oncology.
Real-life example: As per 2025 research, AI-powered robotic surgical systems like Da Vinci have reduced surgical errors by 21% and shortened recovery times by 35%.

7. Better Remote Monitoring and Patient Assistance
AI facilitates continuous remote monitoring via wearables and apps, tracking vital signs and alerting providers to anomalies for timely interventions. Platforms for remote monitoring can also integrate with AI chatbots and agents for decision guidance, alleviating provider workloads while maintaining care quality.
Real-life example: Black Doctor 24/7 platform integrated a clinically tested AI assistant, “Amina,” powered by Infermedica’s engine. Amina triages symptoms and accelerates the diagnostic process by 65%.
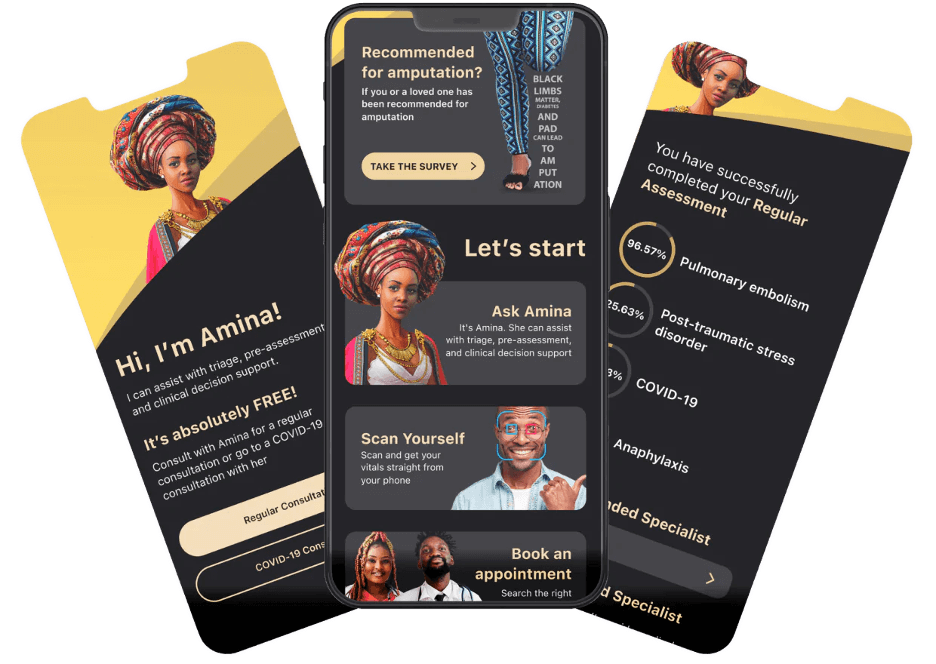
In another instance, implementation of AI-powered Huma’s digital patient platform helped cut readmission rates by 30% and reduced provider workloads by up to 40% through AI monitoring.
8. Integration with Traditional and Mental Health Practices
AI can complement traditional medicine by analyzing ancient texts and identifying medicinal compounds.
Real-life example: India’s traditional knowledge digital library uses AI for Ayurgenomics, exploring treatments for modern diseases. Likewise, in Ghana, researchers are using AI models to help identify and classify medicinal plants. It helped broaden access to holistic care, respect cultural practices, and address global mental health gaps.
And the traditional complementary medicine market is only expected to grow. WHO’s projections show that it will reach $600 billion by the end of 2025, driven by AI innovations, and will continue to grow at 10–20% per year.
What are Risk and Cons of Using AI in Healthcare?
1. High Implementation and Infrastructure Costs
Healthcare AI deployment demands substantial financial investment, often reaching $500,000 for complex solutions. Smaller medical facilities and resource-limited organizations struggle to afford initial setup costs, ongoing maintenance expenses, and necessary infrastructure upgrades.
A survey by HIMSS found that 67% of healthcare organizations cited cost as the primary barrier to AI adoption, with rural hospitals particularly affected by budget constraints.
The financial burden extends beyond initial implementation to include ongoing operational costs such as cloud computing fees, software licensing, staff training, and system maintenance.
Mitigation strategies: Adopt phased implementation approaches starting with pilot programs, leverage cloud-based AI-as-a-Service platforms to reduce upfront capital expenditure, and explore public-private partnerships for shared AI infrastructure costs. For example, implement a tiered deployment strategy like Cleveland Clinic’s AI adoption model, which started with low-cost diagnostic imaging tools before expanding to comprehensive AI suites. It can reduce initial investment by 60% while demonstrating ROI to stakeholders before major capital commitments.
However, Riseapps offers flexible pricing models for MVP development and provides cost-effective quotes through our AI estimation tool. Get instant rough estimates in 60 seconds to plan budgets accurately while avoiding weeks to final calculations.
2. Critical Data Privacy and Security Vulnerabilities
Healthcare AI systems create unprecedented privacy vulnerabilities through large-scale sensitive data collection that attracts cybercriminals targeting valuable protected health information. In February 2025, American medical billing giant Episource notified its 5.4 million customers about a data breach in which their sensitive information was stolen.
Advanced re-identification techniques can compromise anonymized patient data used in AI training, especially as technology capabilities evolve. Third-party cloud platforms and AI developers introduce additional security vulnerabilities through improper data sharing and inadequate consent processes.
Mitigation strategies: Implement zero-trust security architectures, use federated learning to train models without centralizing data, and establish comprehensive patient consent frameworks for AI data usage. For example, implement a zero-trust framework and context-aware model like ZTCloudGuard, that scores authentication requests based on user identity, device, and task to minimize medical errors and reinforce trust chains in distributed healthcare systems.
Riseapps specializes in building HIPAA-compliant healthcare solutions with enterprise-grade security architectures. We conduct comprehensive compliance audits and implement zero-trust security frameworks that protect sensitive patient data throughout the AI development lifecycle.
3. Lack of Transparency in Decision-Making
Healthcare AI operates through “black box” algorithms that cannot explain their diagnostic reasoning or treatment recommendations to clinicians or patients.
A regular review of clinicians’ responses to Explainable Artificial Intelligence (XAI) tools found that 57% of medical imaging studies reported a significant increase in clinician trust when explanations were provided.
The lack of transparency undermines informed consent principles and erodes both clinician and patient trust in AI-assisted medical care.
Mitigation strategies: Develop explainable AI (XAI) models (like IBM’s AI Explainability 360 toolkit) that provide reasoning for clinical decisions, create standardized documentation requirements for AI-assisted diagnoses, and establish transparency mandates for clinical AI systems.
Through our AI consulting expertise, Riseapps develops explainable AI architectures that provide transparent decision pathways and clinical reasoning documentation. We ensure healthcare providers can understand, validate, and communicate AI-driven recommendations effectively.
4. Systemic Bias and Health Equity Deterioration
AI systems perpetuate historical healthcare disparities by training on biased datasets that reflect systemic inequalities in medical care delivery.
For example, risk prediction algorithms have underestimated Black because less money was historically spent on Black and Mixed-raced patients due to access barriers.
Skin cancer detection tools demonstrate reduced accuracy for darker skin tones (84.5% accuracy compared to 93.5% accuracy for white skin tone) when training datasets predominantly feature lighter-skinned patients.
Mitigation strategies: Develop diverse training datasets representing all demographic groups, implement bias detection algorithms during model development, and establish equity auditing protocols for AI deployment. One of the examples of deliberately assembling a broadly representative training corpus for medical AI is Paige AI.
The company built the Virchow foundation model for computational pathology using a 3-million-slide dataset from 800+ labs across 45 countries, explicitly calling out geographic and lab-level diversity as part of model design to reduce dataset bias and improve generalisability.
Riseapps will help you implement bias detection protocols and develop diverse training datasets that ensure equitable AI performance across all patient populations.
5. System Integration and Workflow Disruption
AI tools often slow healthcare delivery rather than improve efficiency due to poor integration with existing clinical workflows and electronic health record (EHR) systems. Therefore, AI implementations may fail because they don’t address real clinical needs or stakeholder requirements. The 2025 research found that 58% of healthcare AI projects failed within the first 18 months due to workflow incompatibility and user resistance.
The disruption occurs when AI systems require clinicians to navigate multiple interfaces, duplicate data entry, or alter established clinical routines without clear benefits. Many AI tools are developed in isolation from actual healthcare environments, resulting in solutions that work in laboratory settings but create friction in real-world clinical practice where time constraints and patient safety are paramount.
Mitigation strategies: Conduct comprehensive workflow analysis before AI deployment, involve end-users throughout the development process, and implement gradual rollouts with continuous feedback loops to refine system integration. For example, adopt a user-centered design approach like AI integration methodology, which embeds clinical staff in development teams from day one and uses rapid prototyping cycles to ensure AI tools seamlessly fit existing workflows.
With proven expertise in multi-EHR integrations including Epic, Cerner, and Athena systems, Riseapps ensures seamless workflow integration through extensive stakeholder engagement, user testing protocols, and comprehensive training programs.
6. Regulatory Uncertainty and Compliance Challenges
Healthcare AI faces unclear regulatory frameworks as agencies struggle to assess continuously evolving algorithms that adapt post-deployment. The absence of standardized approval processes delays beneficial technology adoption while creating legal ambiguity around AI-assisted medical decisions.
The adaptive nature of continuously learning AI systems creates regulatory challenges that traditional medical device approval processes cannot address effectively. Legal liability remains unclear when AI errors occur, with responsibility disputed between developers, healthcare providers, and institutions. This regulatory void delays innovation while creating confusion about safety standards and accountability frameworks.
Mitigation strategies: Establish international AI safety standards like FDA’s Digital Health Center of Excellence pathway for AI device approval, create regulatory sandboxes for AI testing, and develop clear legal frameworks defining responsibility chains for AI-assisted medical decisions.
With 8+ years of healthcare AI experience, Riseapps’ compliance and tech audit services ensure healthcare organizations meet evolving regulatory requirements and complex approval processes.
7. Data Quality and Accessibility Fragmentation
Healthcare AI requires comprehensive, high-quality datasets that often remain fragmented across incompatible systems and organizations. Poor data quality reduces AI accuracy while insufficient data leads to unreliable predictive performance.
Healthcare data remains siloed across incompatible systems, preventing AI algorithms from accessing comprehensive patient information needed for accurate predictions while creating security vulnerabilities.
About 49% of healthcare leaders reported that patient data is stored in fragmented, siloed systems. Almost half of them (47%) also believe healthcare data silos significantly hamper operational efficiency and patient safety due to incomplete information.
Also, patients often lack understanding of how their personal health data is collected, processed, and shared with AI systems, making truly informed consent difficult to achieve.
Mitigation strategies: Adopt interoperability standards like FHIR, develop transparent consent processes with clear explanations of AI data use, and create patient-controlled data sharing mechanisms.
For example, you can use data-sharing platforms like S3PHER, that have advanced encryption (proxy re-encryption, searchable encryption, homomorphic encryption) to let patients control who accesses their health information. It supports secure sharing without centralized consent, aligned with GDPR/HIPAA.
Riseapps’ legacy system modernization services and data integration expertise help healthcare organizations consolidate fragmented data sources while ensuring data quality standards for reliable AI performance.
8. Alert Fatigue and Clinical Decision Overload
AI-powered clinical alert systems generate excessive false positive warnings that overwhelm healthcare providers and reduce responsiveness to genuine critical notifications. This alert fatigue causes clinicians to ignore or dismiss important warnings while creating workflow inefficiencies. High false positive rates undermine trust in AI-generated recommendations.
Healthcare professionals develop excessive trust in AI recommendations, potentially overriding critical clinical judgment when systems fail to account for rare or complex conditions. AI-powered alert systems create “alert fatigue” through high false-positive rates, causing providers to ignore or dismiss warnings that could include valid critical notifications.
As per 2025 research, 90–99% of alarms in clinical settings are false or non-actionable. As a result 70–80% of nurses experience alarm fatigue regularly, leading to slower alert responses and 45% of critical alerts being missed.
Mitigation strategies: Design AI as decision support rather than replacement, implement alert optimization to reduce false positives, and maintain clinician training in independent diagnostic reasoning. For example, Epic introduced alert optimization programs that reduced false positives by 60%.
Through intelligent triage system development and alert optimization services, Riseapps creates AI solutions that minimize false positives while maintaining high sensitivity for critical events. We develop apps that use advanced filtering algorithms and contextual analysis to deliver only actionable, relevant clinical insights.
What are Key Benefits of AI in Healthcare?
Accurate Predictive Analytics and Risk Assessment
Key benefits: AI in healthcare transforms disease prediction through sophisticated data analysis. With artificial intelligence, healthcare providers can identify critical conditions during routine appointments without specialized equipment or lengthy procedures.
Real-world impact: Imperial College London researchers recently unveiled game-changing technology at the European Society of Cardiology conference. Their AI-enhanced stethoscope, developed with Eko Health, processes both ECG signals and heart sounds through cloud-based analysis.
Clinical trial results speak volumes:
- Heart failure detection: 2× higher identification rates
- Atrial fibrillation: 3× more accurate diagnosis
- Heart valve disease: Nearly 2× improved detection
The entire analysis completes in just 15 seconds. This speed enables rapid intervention in primary care settings, potentially saving countless lives through early detection.
Enhanced Diagnostics and Disease Prevention
Key benefits: AI in healthcare revolutionizes infectious disease surveillance by analyzing social media data and web trends to predict outbreaks before they spread. Public health agencies can forecast disease hotspots weeks before traditional surveillance methods detect them.
Real-world impact: Melbourne Sexual Health Centre launched MySTIRisk in 2024, a web-based AI tool that calculates personalized risk scores for HIV, syphilis, gonorrhea, and chlamydia using behavioral and clinical data.
Clinical results demonstrate remarkable precision:
- For HIV, the high-risk cutoff was 0.56 (86% sensitivity, 65.6% specificity), classifying 35% of patients as high-risk and capturing 86% of cases.
- Syphilis had a 0.49 cutoff (77.6% sensitivity, 78.1% specificity), capturing 78% of cases,
- Gonorrhea a 0.52 cutoff (78.3% sensitivity, 71.9% specificity), capturing 78% of cases,
- High-risk groups showed significantly higher odds of positivity (12.3 for syphilis, 9.2 for gonorrhea, 3.9 for chlamydia) compared to average-risk groups.
The system processes patient information in seconds, delivering instant risk assessments and testing recommendations. This enables healthcare providers to offer evidence-based counseling while public health officials gain unprecedented outbreak prediction capabilities.
Faster and Personalized Treatment Planning
Key benefits: AI transforms healthcare decision-making by processing vast amounts of clinical data, learning from patient responses and caregiver feedback, analyzing patient histories, symptoms, and medical guidelines simultaneously. With AI-driven solutions, medical professionals can generate highly personalized treatment plans in minutes rather than hours while maintaining clinical accuracy.
Real-world impact: A U.S.-based healthcare practice developed an advanced dementia care platform using AI-driven personalized care plans. The system employs Large Language Models with Retrieval-Augmented Generation to analyze patient medical histories, symptoms, and caregiver input, generating dynamic treatment recommendations for the 7 million Americans living with Alzheimer’s dementia.

Clinical results demonstrate significant efficiency gains:
- Treatment plan generation: Reduced from 4 hours to 30 minutes (84% time savings)
- Care plan accuracy: Projected 20-30% improvement in personalized recommendations
- Documentation efficiency: 50% reduction in manual note-taking through AI transcription
- Target AI accuracy: 85% for care plan recommendations post-launch
The platform integrates real-time voice transcription, automated medical documentation, and AI-powered alerts for critical events like fall risks. This comprehensive approach addresses the complex needs of dementia patients while supporting the 83% of caregivers who report high emotional stress.
Cross-Geographical Surgical Precision
Key benefits: AI-powered robotic surgery enhances surgical accuracy while enabling remote mentorship. AI systems provide surgeons with real-time data analysis, procedural recommendations, and educational support regardless of geographical distance. With these solutions, healthcare experts can access expert guidance instantaneously during complex procedures, being miles away.
Real-world impact: Orsi Innotech’s Surgical AI & Telesurgery Days 2025 in Ghent showcased groundbreaking innovations that demonstrated AI’s surgical potential.
Revolutionary demonstrations include:
- ChatGPT-integrated surgery: First robot-assisted procedure with real-time AI assistance (developed with NVIDIA)
- Belgium-Shanghai telesurgery: Remote operation using Toumai surgical robot across continents
- Live audience interaction: AI answers surgical questions during actual procedures at AZORG Ziekenhuis
Meanwhile, the Belgium-Shanghai connection demonstrates how telesurgical techniques eliminate geographical barriers in specialized care.
24/7 Health Support
Key benefits: The AI-powered tools give people access to immediate mental health support without barriers like appointment scheduling, insurance requirements, or fear of stigma. The AI in mental health offers consistent, evidence-based guidance whether users are between therapy sessions, exploring self-care independently, or experiencing crisis moments.
Real-world impact: Ava Mind provides 24/7 mental health support through AI-powered conversations without requiring sign-ups or personal data collection. The platform processes over 1 million requests monthly while maintaining complete user privacy and anonymity.

Clinical capabilities demonstrate broad accessibility:
- CBT-trained responses: AI delivers evidence-based therapeutic techniques instantly
- Privacy-first design: No account creation, tracking, or data storage required
- 24/7 availability: Immediate support during crisis moments or routine mental health maintenance
- 65,000+ messages: Processed monthly showing high user engagement and trust
The system enables users to explore emotions without judgment while building personalized wellness libraries for ongoing support. Premium features include voice chat for hands-free interaction, creating a more human-like therapeutic experience.
Economic Efficiency and Cost Reduction
Key benefits: AI accelerates healthcare economics by optimizing treatment selection, early disease detection, and streamlining clinical workflows. AI-driven systems help analyze vast patient datasets to identify cost-effective interventions while reducing expensive late-stage complications through predictive modeling and personalized care approaches.
Real-world impact: A comprehensive Danish study analyzed over 249,000 screening mammograms to evaluate AI’s cost-reduction potential in breast cancer screening. The research tested three AI integration models to address radiologist shortages while maintaining diagnostic accuracy.
Economic results demonstrate substantial savings:
- Workload reduction: 48-50% fewer mammograms requiring human review across all scenarios
- AI as first reader: 48.8% screening reduction while maintaining cancer detection rates
- AI triage system: 49.7% workload reduction with improved diagnostic accuracy
- Cost efficiency: Nearly 50% reduction in labor costs for mammography interpretation
The AI triage approach proved most effective, sorting cases into low-risk (no review needed), high-risk (immediate attention), and moderate-risk (human review required) categories.
This system addresses mounting healthcare pressures from radiologist shortages and increasing screening demands.
10 Best Practices for Effective AI Implementation in Healthcare
With increased AI adoption in healthcare, organizations must address implementation challenges strategically. Our 10 recommendations provide a framework for deploying AI to enhance patient care while managing risks.
- Establish AI governance. Assemble a team with IT, data science, executive, and bioethics expertise to review proposals from stakeholders, identifying AI solutions for inefficiencies or targeted problems.
- Define objectives and expectations. Evaluate if AI is necessary or if rule-based alternatives suffice; select appropriate AI types (e.g., generative or neural networks) and decide on building versus buying based on internal capabilities.
- Evaluate vendors thoroughly. Use formal RFPs and resources like the Coalition for Health AI registry and involve business units to ensure workflow alignment.
- Safeguard data privacy. Deploy foundational models locally to fine-tune with secure, proprietary data, balancing training needs with anonymization challenges and avoiding external data sharing.
- Start with high-impact use cases. Prioritize applications like administrative automation (e.g., note transcription, EHR analysis) or value-based care support to achieve early successes and optimize resource allocation.
- Collect stakeholder feedback regularly. Hold routine discussions on AI performance, accuracy, and impact. Integrate this review process into organizational culture to adapt to expanding AI applications.
- Uphold ethical standards.Ensure systems are reliable, bias-monitored (distinguishing justified from unintended biases), and transparent, with patient opt-out options and considerations for vulnerable groups.
- Validate and monitor models. Conduct internal and external reviews of implementation, data inputs, and outputs; leverage in-house testing for advanced models to address institution-specific variations.
- Provide training and support. Guide users in assessing tool suitability for patients or processes; promote transparency on model training and encourage critical evaluation of outputs.
- Recognize AI limitations.Train users to override fallible AI decisions, contrasting with validated diagnostics, and assess error consequences.
How Riseapps Can Help Maximize Advantages of AI in Healthcare?
Riseapps combines deep healthcare knowledge with AI expertise to ensure your project’s success from strategy to implementation. We are also trusted by multiple Fortune-500 healthcare organizations and innovative digital health startups worldwide.
We offer full-cycle AI consulting & development services for healthcare providers including:
- AI strategy consulting aligned with your healthcare delivery models.
- Generative AI development for workflow automation and personalized patient communications.
- AI chatbot & AI virtual assistant development for patient support, engagement and 24/7 automated communication.
- Integration of advanced AI capabilities into existing EHR, telehealth platforms and clinical workflows.
With Riseapps, you’re not just getting technology. You’re investing in an AI partner for your long-term success.
FAQ
What are the pros and cons of using AI in healthcare?
Pros of using AI in healthcare: Faster diagnosis, improved accuracy, reduced costs, 24/7 availability, pattern recognition in medical imaging, drug discovery acceleration. Cons of using AI in healthcare: Privacy concerns, potential bias, high implementation costs, lack of human empathy, regulatory challenges, job displacement fears.
What are the 5 pros and 5 cons of AI?
5 pros of AI in healthcare: 1. Boosts efficiency in tasks. 2. Advances healthcare diagnostics. 3. Automates repetitive jobs. 4. Enhances data analysis. 5. Improves accessibility tools. 5 cons of AI in healthcare: 1. Causes job displacement. 2. Raises privacy concerns. 3. Perpetuates biases. 4. Enables misuse like deepfakes. 5. Poses ethical dilemmas.
What are the 4 advantages and 4 disadvantages of AI?
Advantages of AI: It automates repetitive tasks, enhances decision-making with data analysis, reduces human error, and provides 24/7 availability. Disadvantages of AI: It can cause job displacement, has high implementation costs, lacks true creativity and empathy, and raises ethical concerns like bias and privacy.
What are the benefits of AI in healthcare?
AI enhances healthcare by enabling faster, more accurate diagnostics, personalizing treatment plans, and streamlining administrative tasks. This leads to earlier disease detection, improved patient outcomes, and increased operational efficiency.
Contact Us









