EHR Software Development: How to Build a Scalable and 100% Compliant EHR System in 2025

Deloitte US Center for Health Solutions has discovered that 70% of surveyed healthcare executives mentioned improving operational efficiency and productivity gains as their top priorities in 2025. And 60% of respondents emphasized the need to invest in EHR and EMR solutions to achieve those priorities.
Take The Wound Pros, a Riseapps-developed EHR system for wound care specialists. The custom solution:
- cuts patient care delivery costs.
- streamlines patient management.
- ensures 100% compliance with HIPAA & CMS requirements.
The result? A cross-platform interoperable solution featuring 120+ wound care management modules designed to centralize data for thousands of patients efficiently. Thus, the system significantly reduces physicians’ administrative workload. This is the power of a well-built EHR platform.
Our guide covers everything you need to know about the EHR software development process in 2025 — from essential features and compliance regulations to development costs and real-world implementation strategies.
EHR vs. EMR system: Choosing the right one for your healthcare business
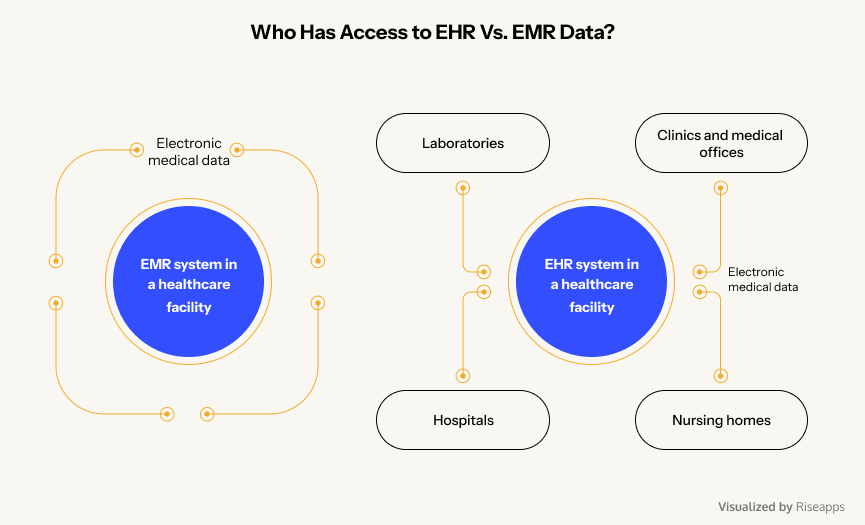
A common misconception is that electronic health record (EHR) and electronic medical record (EMR) systems are the same. While both digitize patient information, their scope, accessibility, and functionality differ. Here’s how:
What’s the difference?
- EMR: A digital version of paper charts, used within a single healthcare facility to record diagnoses, treatments, billing, care coordination, telehealth integration, and medical history. Primarily designed for internal use by a doctor or clinic.
- EHR: A comprehensive digital system that integrates patient data across multiple providers, hospitals, and labs, allowing seamless information exchange.
Who uses them?
- EMRs are limited to one practice or facility—think of them as a hospital’s in-house medical record system.
- EHRs provide a broader, interconnected view of a patient’s health, accessible to clinics, hospitals, specialists, laboratories, and even patients for better coordination of care.
Which one should you choose?
- For small practices that need basic patient record-keeping, an EMR may be sufficient.
- For hospitals, multi-specialty clinics, and networks aiming for interoperability and seamless patient care, an EHR is the better choice.
If you’re looking for a scalable, future-proof solution, EHRs offer better long-term value by enabling integrated, patient-centered healthcare with broader accessibility.
Unlike electronic health record platforms, EMR solutions are designed solely for internal use, so data cannot be easily shared between facilities.
EHR market size, segments, and factors shaping it
As of 2024, the global EHR market is valued at $28.60 billion and is projected to reach $43.66 billion by 2034, growing at a CAGR of 4.32% (Towards Healthcare). In the United States, the EHR market size was estimated at $11.38 billion in 2023, with an expected CAGR of 2.24% through 2030 (Grand View Research).
Market segments
The EHR market is categorized based on product type, application, and geographical region:
By product type:
- On-premises EHR systems. Installed locally on hospital servers, offering greater control but requiring substantial upfront investments and maintenance.
- Cloud-based EHR systems. Hosted on external servers, providing scalability and reduced IT costs, such systems face increasing adoption due to flexibility and remote accessibility. In 2023, cloud-based systems captured 48% of the EHR market (GlobeNewswire).
By use cases:
- Clinical applications. Include patient management, electronic prescribing, and clinical decision support systems. Clinical applications lead the market, holding a 46% share (GlobeNewswire).
- Administrative applications. Encompass scheduling, billing, and compliance management.
- Reporting applications. Focus on regulatory reporting and quality management. Reporting in healthcare systems is projected to see the fastest growth, with a 5.1% CAGR by 2033 (Towards Healthcare).
By regions:
- North America holds the largest market share, attributed to advanced healthcare infrastructure and supportive government initiatives. In 2023, North America led the global market with a 46% share (Precedence Research).
- Europe experiences steady growth with increasing digitalization in healthcare. The European Union’s program of ensuring 100% of EU citizens have access to electronic health records by 2030 is steadily progressing. The most recent score among European countries is 79% as of 2024 compared to 72% in 2023 (Digital Decade 2024 by European Commission).
- Asia-Pacific is anticipated to witness the fastest growth due to expanding healthcare facilities and IT infrastructure. The Asia-Pacific EHR market is expected to grow at a CAGR of 5.06% from 2023 to 2033. (Spherical Insights) The Ministry of Health Singapore has announced that in 2025 all private hospitals will connect to the National EHR system to facilitate unhindered exchange of patient data (Healthcare IT News).
Factors shaping the EHR and EMR market
Digital breakthroughs
Integration of AI and ML enhances data analytics, predictive modeling, and clinical decision support, leading to improved patient outcomes. Harvard Medical School’s AI model, “Chief,” has achieved up to 94% accuracy in diagnosing various cancers by analyzing digital tumor slides, outperforming existing diagnostic methods by up to 36%. A projected reduction in treatment costs using AI for diagnoses is 50% according to the Harvard School for Public Health.
Data security and privacy concerns
The increasing digitization of health records requires robust cybersecurity measures to protect sensitive patient information, influencing EHR/EMR system designs and regulatory compliance. For instance, a ransomware attack on Ascension Health in 2024 led to an electronic health record system outage for almost 4 weeks (HIPAA Journal: The Biggest Healthcare Data Breaches of 2024). The provider confirmed that hacking groups got access to the protected health information of 5,599,699 patients in total by 2025.
Healthcare workforce dynamics
While EHRs and EMRs aim to streamline operations, studies have shown that improper implementation can lead to increased administrative burdens and workplace stress among healthcare staff, affecting overall efficiency. In November 2022, Central Norway introduced Epic’s “Helseplattformen” system. Within two months, approximately 25% of doctors at the region’s main hospital considered resigning, and 40% experienced stress-related health issues attributed to the new IT system (NPK).
Patient safety and quality of care
Proper adoption of EHR and EMR systems leads to enhanced patient safety, improved clinical decision-making, and reduced medication errors, thereby elevating the quality of care. The BMC Nursing study revealed that the implementation of EMR reduces errors in drug administration and nursing workload management by 30%.
Out-of-the-box software vs. custom EHR solutions
One of the biggest decisions when implementing an EHR system is whether to buy a ready-made solution or invest in a custom-built platform. While off-the-shelf EHR software may seem like the quickest and most affordable option, it often lacks flexibility and scalability. On the other hand, custom solutions provide tailored functionality but come with a higher upfront investment. Let’s break down the pros and cons of both approaches to help you make the right decision.
Out-of-the-box EHR software
Off-the-shelf EHR software is pre-configured and ready to use immediately after installation and onboarding sessions (up to 2 weeks on average).
Core benefits
- Lower upfront costs. Ready-made solutions typically have lower initial expenses compared to custom-built software.
- Faster onboarding. Since the software is pre-built, installation and basic configuration are the only steps required before it becomes operational.
- Built-in support and updates. Vendors provide customer support, security patches, and software updates, ensuring compliance with industry standards.
Key downsides
- Limited customization. May not fully align with your organization’s specific workflows, requiring workarounds.
- Hidden costs. Licensing fees, upgrades, and ongoing maintenance expenses can add up over time.
- Scalability concerns. Standard EHRs may not support complex integrations or long-term business growth, leading to eventual replacement needs.
What are the key players in the EHR market?
According to the Definitive Healthcare Atlas Technology Install Dataset, the top hospital EHR vendors have the following market share in the US:
- Epic Systems Corporation – 37.7%
- Oracle Cerner – 21.7%
- MEDITECH – 13.2%
- Evident Health (by CPSI) – 6.9%
- Altera Digital Health (by Harris) – 3.4%
Customized EMR/EHR platforms
A custom-built EHR system is developed from scratch to meet an organization’s specific operational, compliance, and workflow needs.
Core benefits
- Tailored to your needs. Custom development allows you to build exactly what your organization requires, avoiding unnecessary features.
- Scalable and future-proof. The software architecture can grow with your organization, supporting new integrations and expansions as needed.
- Long-term cost efficiency. While the initial investment is higher, custom EHRs eliminate recurring licensing fees associated with off-the-shelf solutions.
- Competitive advantage. A well-optimized system improves efficiency, enhances patient data management, and gives you a technological edge over competitors.
- Direct control over updates and improvements. Unlike commercial EHRs, custom systems allow quick implementation of new features, rather than waiting for vendor updates.
Key drawbacks
- Higher initial costs. Custom EHR software development requires a larger upfront budget to design, build, and implement.
- Requires ongoing maintenance. Unlike off-the-shelf software, custom EHRs need dedicated IT teams for support, updates, and security management.
5 core drivers to build your own EHR/EMR system
Let’s review the major benefits of developing and implementing EHR and EMR solutions.

Enhanced clinical decision-making
EHR software can help clinicians exchange patient data across several hospitals, nursing homes, states, and countries. Remote and 24/7 access to patient’s health records allows doctors to make better and faster decisions on diagnosis and treatment. Thus, EHR adoption translates into safer care. Northern Light Health (Maine) fine-tuned its medication-alert system in the EHR, which led to a 71% reduction in medication errors (from ~7 to ~2 errors per 100 orders) (Oracle).
Improved healthcare providers’ workflow
EHR systems automate various administrative processes, including form filling, allowing doctors to focus on patients. Plus, patients can schedule online appointments via patient portals and telemedicine functionality, eliminating the need for phone calls and in-person visits.
To give you an example, M Health Fairview (an integrated health system in Minnesota) implemented a crowdsourced EHR optimization program that yielded major efficiency gains such as reduced documentation burden and improved EHR usability, translating to roughly 5 minutes of clinician time saved per hour (about 20 minutes saved per provider per day) (National Library of Medicine).
Improved patient outcomes
EHR systems allow patients to access their medical records, schedule appointments, and simplify doctor-patient cooperation. Timely medical interventions can be life-saving, particularly for at-risk patients. For instance, a community hospital in Vermont reported a 60% decrease in near-miss medication events and a 20% increase in the completion of daily fall assessments after implementing an EHR system (HealthIT).
Lower readmission rates
Advanced functionality within an EHR system helps clinicians provide timely interventions for at-risk patients and efficiently coordinate follow-up care. For example, Northern Light Health used EHR-based risk scoring and care management to lower cardiac patients’ readmissions. In 18 months, overall cardiac-related readmission rates fell from 9.8% to 9.1%, and heart failure readmissions dropped from 17% to 14.5% (Oracle).
Personalized care
EHR software allows healthcare providers to build holistic patient profiling and automate patient data management and analysis. With a clear dashboard of patient’s vitals, clinicians can compose personalized treatment plans. Documenting and analyzing cancer prevention measures and pre-cancer genome atlas in the EHR for at-risk patients can potentially prevent 40% to 50% of cancers (National Library of Medicine).
How to build an EHR system: 10 crucial steps to succeed
By following this step-by-step roadmap on how to develop EHR, healthcare providers can build a scalable, future-proof EHR solution that enhances patient care, operational efficiency, and regulatory compliance.
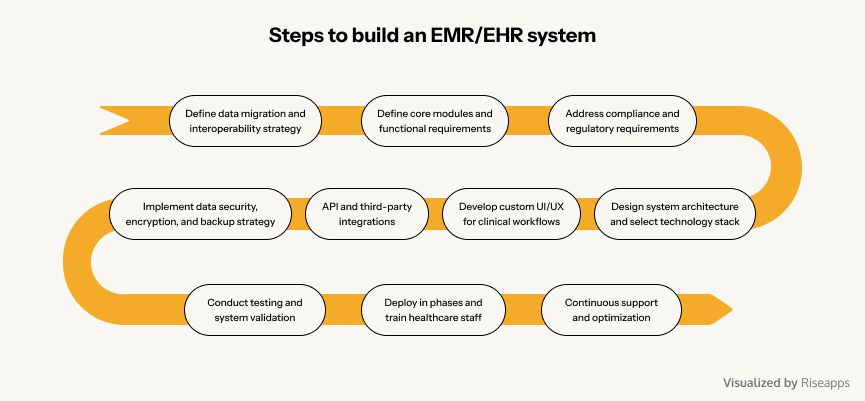
Step 1: Define data migration and interoperability strategy
Before development begins, establish with your EHR software development company a clear strategy for handling patient data migration from legacy systems. Ensuring seamless interoperability between healthcare providers, pharmacies, insurance systems, and third-party apps is critical. Critical substeps include:
- identify legacy records for migration
- implement FHIR and HL7 standards for interoperability
- develop data mapping strategies for seamless integration
- ensure compliance with HIPAA, GDPR, and other regulations governing patient data exchange
Why it matters: Without proper interoperability, you risk having data silos in your EHR/EMR system, preventing healthcare professionals from accessing critical patient information when needed.
Step 2: Define core modules and functional requirements
Clearly outline features before EHR software development, based on clinical workflows, patient needs, and administrative tasks. To simplify this process, hire an experienced team that knows how to create an electronic medical record system to efficiently prioritize features for Phase 1 (MVP), and plan for future expansion.
Why it matters: Customizing features from the beginning ensures your EHR system fits your organization’s unique needs, rather than forcing providers to adapt to rigid, prebuilt solutions. Discuss your goals, needs, and functional and non-functional requirements to help your team understand how to create EHR software that fits your business model.

E-prescribing and order entry
E-prescribing allows doctors to send prescriptions to pharmacies as quickly as possible. It saves time and eliminates human error. The module includes subfeatures such as prior electronic approval, interaction, event alerts, medication decision support, and more.
Appointment scheduling
Implementing basic appointment scheduling during EHR system development allows doctors to see their appointments, manage waitlists and no-shows, and reschedule them.
Compliance tracking
Consider this functionality for monitoring essential practice operations and ensuring that they are carried out according to healthcare sector rules and regulations during the EHR system development.
Clinical dashboard
The dashboard displays key practice performance indicators, providing a comprehensive picture of healthcare practice. Data from the practice analysis can be tabulated or graphical. This helps doctors and other healthcare providers to detect negative patterns and act quickly.
Task management
Doctors and other healthcare professionals can use task managers to access all of their most frequently used features in one place, making it easier to manage their day-to-day operations. Interactions with patients can take the form of video, audio, text, chat, or visuals.
Patient history and profile
EHR software stores patient’s clinical data, including their medical history and health issues. Doctors may also require such data as demographics, patient location, vital signs, medications, treatment, and laboratory notes.
EHR system features for patients:
Patient portal
Most electronic health record technology includes a patient portal through which patients can schedule appointments, communicate with their doctor, receive test results and prescriptions, and pay for medical services.
Telemedicine and virtual consultations
Built-in video conferencing allows patients to consult with doctors remotely for follow-ups, reducing unnecessary hospital visits.
Wearable Integration
Syncing EHR software with wearable health devices (e.g., smartwatches, glucose monitors) to track vitals like heart rate, oxygen levels, and blood pressure.
Family health management
Caregivers can manage dependents’ health records, schedule appointments for family members, and monitor elderly patients’ medical conditions.
Step 3: Address compliance and regulatory requirements
During electronic health record development, you must ensure an EHR system complies with industry standards, laws, and regulations, governing PHI security and privacy.
- HIPAA and HITECH (US). Data encryption, patient consent, access controls.
- GDPR (Europe). Data portability, consent-based data collection.
- FDA and MDR. If your EHR integrates with medical devices, ensure it meets device software regulations.
- ONC and CMS Certification. Required for EHRs participating in Medicare and Medicaid incentive programs.
Why it matters: Non-compliance can lead to financial penalties, lawsuits, and reputational damage.
Step 4: Design system architecture and select technology stack
Choose a scalable, secure, and high-performance system architecture for building an EHR system that supports real-time data processing, cloud capabilities, and seamless third-party integrations.
- Backend: Java, Python, Node.js with microservices architecture.
- Frontend: React, Angular, or Vue.js for a user-friendly interface.
- Database: PostgreSQL, MongoDB, or Firebase for secure health data storage.
- Hosting: Cloud-based (AWS, Azure, Google Cloud) or on-premises infrastructure for better control.
Why it matters: A flexible tech stack ensures your EHR can scale, integrate with new technologies, and comply with evolving healthcare standards.
Step 5: Develop custom UI/UX for clinical workflows
User experience (UX) in EHR development is critical for both clinicians and patients to ensure seamless adoption and efficient workflows.
- Design intuitive dashboards for faster patient record access.
- Optimize EHR forms and documentation processes to reduce manual work.
- Ensure mobile-friendly interfaces for remote access via smartphones or tablets.
- Implement role-based access for security (doctors, nurses, admin staff).
Why it matters: Poorly designed EHRs lead to physician burnout. A well-structured UI improves efficiency, reduces time spent on documentation, and enhances user satisfaction.
Step 6: API and third-party integrations
To maximize efficiency and interoperability, integrate your EHR with existing healthcare ecosystems.
- Laboratory and imaging software (LIS, PACS) for automatic syncing of lab test results.
- Pharmacy and e-prescriptions (eRx) to create and send medical prescriptions electronically.
- Billing and insurance (RCM, HL7 Claim Processing) to streamline claims and payments.
- Wearable and IoMT devices to collect and exchange patient vitals in real time.
Why it matters: Without API integrations, your EHR will struggle to function in modern healthcare settings, leading to workflow inefficiencies and manual data entry.
Step 7: Implement data security, encryption, and backup strategy
Security is non-negotiable in healthcare software. Implement robust security measures to protect patient data:
- End-to-end AES-256 encryption for data in transit and at rest.
- Multi-factor authentication (MFA) and role-based access control (RBAC).
- Automated data backup and disaster recovery for high availability.
- Real-time security monitoring and threat detection.
Why it matters: Cyberattacks on healthcare systems are increasing — one breach could expose millions of patient records. Proactive security measures ensure compliance and prevent costly legal issues.
Step 8: Conduct testing and system validation
Before launching, rigorous testing is required to eliminate security vulnerabilities, performance issues, and interoperability failures.
- Unit and integration testing ensures all features work independently and in sync.
- Penetration testing identifies security gaps to prevent data breaches.
- Usability testing confirms UI/UX meets clinician and patient needs.
- Performance and load testing guarantees fast response times and high reliability.
Why it matters: A single bug in an EHR can delay treatments, misfile prescriptions, or cause compliance issues. Testing prevents operational failures.
Step 9: Deploy in phases and train healthcare staff
Rolling out an EHR system gradually helps prevent disruptions in patient care.
- Pilot launch in one department before full-scale deployment.
- Provide role-based staff training on using the EHR effectively.
- Offer ongoing support and user feedback channels to address concerns.
Why it matters: Ensuring proper onboarding improves user adoption and satisfaction.
Step 10: Continuous support and optimization
After deployment, regular updates, security patches, and feature enhancements are necessary for long-term system efficiency.
- Set up real-time monitoring to track EHR performance.
- Address bug fixes and compliance updates proactively.
- Expand features based on clinician and patient feedback.
- Plan for scalability to ensure the system grows with new integrations and user demand.
Why it matters: A well-maintained EHR system remains compliant, secure, and optimized for evolving healthcare standards.
HIPAA compliance in EHR/EMR development: What you need to know
Since EHR and EMR solutions handle sensitive patient health information (PHI), these systems must comply with federal laws such as HIPAA to ensure data security and privacy.
Why HIPAA compliance matters in EHR development
Failure to meet HIPAA standards can lead to hefty fines, legal action, and loss of trust. Implementing secure authentication, access control, data encryption, and compliance auditing is non-negotiable when building an EHR or EMR system.
Building standards-compliant EHR/EMR system
To build an interoperable EHR software, it is critical to study industry-specific standards:
- HL7: Transfers documents between healthcare systems to fulfill a request. This ability to exchange information and move data reduces geographically isolated medical care, allows medical device innovation, and makes patient care safer.
- ICD-10: Death certificates are coded using ICD-10. The World Health Organization publishes and copyrights the classification. WHO has authorized a US government ICD-10 adaptation.
- SNOMED: Systematized medical nomenclature. It is a systematic, computer-processable collection of medical terms, codes, definitions, and synonyms for anatomy, diseases, discoveries, procedures, microorganisms, and substances.
- DICOM: Medical imaging and data management standard.
- LOINC: Health measurements, documents, and observations international standard. LOINC helps hospitals, labs, government agencies, and insurers identify and transfer data.
EHR/EMR system development costs explained
Looking at the costs associated with setup, rollout, and upkeep allows us to calculate an approximate EHR/EMR Total Costs of Ownership (TCO).
Cost of implementing EHR systems
Implementation costs can be difficult to predict, but case studies can help. According to the Health Affairs study, the average cost of implementing an EHR in a multi-physician practice is $162,000, with an additional $85,500 needed for the first year of maintenance. In this case, the team spent 611 hours implementing the EHR system.
Across the 30 primary care practices in the Medical Economics study, an average of $5,900 was spent on hardware, software, peripherals, and network connections to ensure EHR implementation. An additional $3,094 was spent on IT and other outside support by roughly half of the practices.
Cost of maintaining electronic health records
According to the Software Path report, the average budget for EHR maintenance is $1,200 per year per user. For cloud-based systems, the cost breakdown of system maintenance is primarily the responsibility of your EHR system provider. However, you should also take into account the cost of maintaining and ensuring the security of your data through an IT department, the costs of employee support and training, additional server setup, and the cost of extra hardware.
Why hire Riseapps as your EHR development company
At Riseapps, we develop custom EHR and EMR solutions that streamline workflows, enhance patient care, and ensure regulatory compliance. With expertise in Epic, Cerner, AthenaHealth, AllScripts, and SureScripts integration, we help healthcare enterprises and MedTech companies achieve seamless data exchange and interoperability. Our cutting-edge engineering and deep industry experience enable us to build scalable, secure, and future-proof healthcare solutions.
Let’s look at Kego as one example of a HIPAA-compliant healthcare app, among many others.
Customer request
Kego, an on-demand urgent care service, sought to digitally transform its healthcare delivery model by building a HIPAA-compliant mobile and web platform. The company needed:
- A patient-facing mobile app for booking virtual doctor appointments.
- A full-featured web platform for healthcare providers to manage consultations.
- Secure payment gateway integration for seamless billing.
- Telemedicine functionality with video calls and real-time chat.
- Cloud-based storage for medical records while ensuring data encryption and HIPAA compliance.
Solution
Riseapps partnered with Kego to turn their concept into a fully operational health tech product by providing:
- Mobile app development from scratch, enabling patients to schedule virtual visits, store medical records, and connect with doctors.
- Web-based provider platform to manage appointments, consultations, and prescriptions.
- Integrated payment gateway for hassle-free transactions.
- Telemedicine features with high-quality video calls and secure messaging for real-time consultations.
- Cloud-based documentation storage with strong encryption protocols to comply with HIPAA security standards.
Results
- Launched a fully HIPAA-compliant telehealth platform.
- Enabled patients to book, consult, and store records securely in one place.
- Transformed Kego’s business model into a scalable, tech-driven urgent care solution.
- Enhanced doctor-patient interactions via real-time communication tools.
Today, Kego provides a streamlined, secure, and efficient healthcare experience, helping patients access urgent care anytime, anywhere.
FAQ
What are the features of EHR software?
The key features of EHR include appointment scheduling, charting, e-prescribing, a patient portal, HIPAA compliance, and more. Artificial intelligence (AI)-based technologies are a powerful way to improve EHR usability. Third-party solutions can facilitate the transfer and exchange of clinical information.
What is EHR software?
EHR software is designed to help healthcare organizations maximize clinical productivity and enhance the quality of patient care, at the same time streamlining revenue through personalized care delivery.
How long does it take to build an EHR system?
The timeline for EHR development depends on the complexity, features, integrations, and compliance requirements. On average: basic EHR system (patient records, scheduling, e-prescriptions) – 6 to 9 months; mid-range EHR with integrations (lab results, billing, telemedicine) – 9 to 15 months; enterprise-grade EHR (AI-driven analytics, remote monitoring, interoperability) – 12 to 24 months
What are the 5 components of an electronic medical record (EMR) system?
An EMR system consists of five key components: patient data and medical history, clinical decision support (CDS) for alerts and insights, order entry and prescription management, administrative and workflow tools, and interoperability and data exchange for seamless data sharing.
Contact Us








